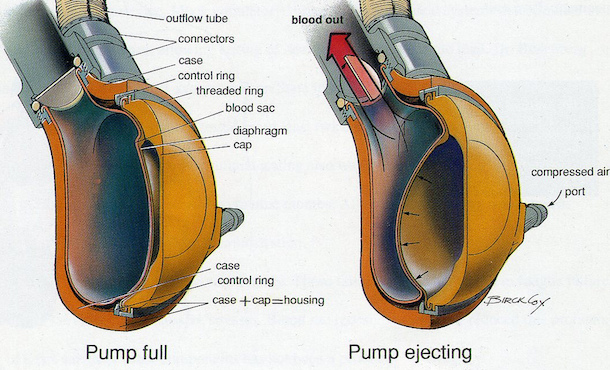
Cross-sectional view of a heart-assist pump. Credit: Penn State
Building a safer heart pump
Focus of $3 million grant on designing a heart pump with lower blood clot, stroke risks
September 4, 2018
UNIVERSITY PARK, Pa. — Blood pumps are increasingly used as a temporary treatment for patients with end-stage heart disease or heart failure while they wait for a heart transplant. But the risk of blood clots and strokes puts patients in peril before they can receive a donor heart, and is a barrier to their use in less sick patients who could benefit from their use.
Solving these issues is the focus of a four-year, $3 million grant from the National Institutes of Health awarded to Keefe Manning, professor of biomedical engineering and surgery, and Gerson Rosenberg, professor of surgery and bioengineering, and chief of the College of Medicine’s Division of Applied Biomedical Engineering. Manning and Rosenberg will use the grant to leverage computational methods to develop both a clot model to predict where clots might form during blood pump use, and methodologies to design safer blood pumps.
“In a small but significant number of patients, bleeding can occur during blood pump use, and in some instances, clots can form in the pumps or tubes leading into and from the heart,” Rosenberg said. “Our research focuses on developing methods to design improved pumps that will have a reduced incidence of bleeding and strokes.”
Manning and Rosenberg hope their research will help develop blood pumps that can be used, for example, on a congestive heart failure patient at a much earlier state in their disease. This would greatly benefit the patient, because if there is a blood pump intervention at a much earlier stage of the disease process, then recovery can occur much sooner. The heart assisted by a blood pump will not have to work as hard, and therefore last longer.
At the same time, a safer heart pump is important for patients with serious heart disease due to the fact they are commonly used as a temporary treatment for patients waiting for a heart transplant. The less time needed to use a heart pump the better, given the stroke and blood clot risk. However, waiting times can last for months because there is an insufficient number of donor hearts available to patients.
According to the United Network for Organ Sharing, as of August 23 there were 1,961 heart transplants during 2018. Also as of August 23, there were 3,939 individuals on the waiting list for a heart transplant. On average more than 25 percent of those waiting for a heart transplant do not live long enough to receive a new heart due to the long wait time.
“The bottom line is the longer a patient can go with a safer blood pump, the higher likelihood they have of finding a donor heart and surviving,” Manning said.
Manning added that Penn State has been an innovator in mechanical circulatory support such as blood pumps, with a nearly 50-year history of developing technology for patients with serious heart disease.
“This research is a continuation of a tradition of collaborative cardiac-related research efforts at Penn State that have a pretty strong track record of success,” Manning said. “Penn State has been very good about translating design and technology research into the clinic for applied use.”
Some of the preliminary data for this proposal was generated through the support of a Huck Institute for Life Sciences seed grant.
MEDIA CONTACT:
Jamie Oberdick
jco11@psu.edu