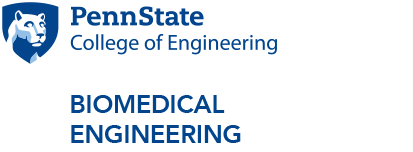
Human stem cell-derived pancreatic cells could be transplanted into diabetic patients to treat or even cure Type 1 diabetes.
Lian receives ENGINE grant for stem cell-based diabetes therapy
3/12/2019
UNIVERSITY PARK, Pa. – Xiaojun “Lance” Lian, assistant professor of biomedical engineering, was one of three recipients of the College of Engineering’s ENGineering for Innovation & Entrepreneurship (ENGINE) grant for his project titled “Small Molecule-Based Definitive Endoderm Kit and Pancreatic Progenitor Kit for Stem Cell Research and Therapy.” The project focuses on differentiating stem cells into pancreatic beta cells to be used for therapies to treat Type 1 diabetes.
The pancreas produces enzymes that help digest food as well as hormones that play an important role in maintaining sugar and salt balance in our bodies. One of those hormones, insulin, is necessary to regulate blood sugar. Beta cells, a type of cell found in the pancreas, synthesize and secrete insulin. Type 1 diabetes disrupts this process.
“With Type 1 diabetic patients, their pancreatic beta cells are destroyed by their own immune cells,” Lian said. “Therefore, they do not have beta cells to control blood sugar concentration for them.”
One solution, Lian noted, is stem cell therapy.
“We could make functional beta cells from stem cells, and then transplant these stem cell-derived beta cells to help these diabetic patients,” he said.
There is a technical hurdle to overcome, however. Currently, there is a lack of robust cell culture systems that efficiently and economically direct stem cell lines to differentiate into populations of functional beta cells.
To solve this issue, Lian’s team discovered a new way for stem cells to differentiate into pancreatic lineages by using small molecules, which are low molecular weight organic compounds that make up most pharmaceutical drugs. The small molecules would activate key cell signaling pathways, an important step in differentiating stem cells into other cells.
“Our new method is an improvement on previous growth-factor dependent methods, which use proteins to stimulate differentiation,” Lian said. “This is due to small molecules being more stable, easy and cheap to manufacture, thus making stem cell differentiation more efficient and cost-effective.”
To generate beta cells from stem cells, specific steps must be followed. Researchers must first differentiate stem cells into definitive endoderm cells. In a very early-development stage human embryo, a definitive endoderm is a germ layer that eventually transforms into organs such as the pancreas, liver and lungs. The Lian lab differentiation mimics this transformation.
Researchers then differentiate the definitive endoderm cells into pancreatic progenitor cells, which are in turn differentiated into beta cells.
“The functional, stem cell-derived beta cells can be transplanted into Type 1 diabetic patients to help them fight the disease,” Lian said.
Using the ENGINE grant, Lian’s lab plans to create small molecule-based stem cell differentiation kits for both definitive endoderm cells and pancreatic progenitor cells. He will then recruit students with cell culture experience to test the kits in his lab. Finally, the kits will be shipped to collaborators at Purdue University and the University of Wisconsin for further testing.
“Completion of this project will hopefully yield two stem cell differentiation kits, which would have immediate potential for broad commercial impact on the treatment of Type 1 diabetes,” Lian said.
The college's ENGINE grants program is supplemented by the Penn State Research Foundation Fund for Innovation, which matches one dollar for every two dollars provided by the college, up to a maximum $75,000 total investment per project.